10+ Esbl Secrets To Reduce Risk Successfully
The rise of Extended-Spectrum Beta-Lactamase (ESBL) producing bacteria has become a significant concern in the medical community, posing a substantial risk to patient health and complicating treatment options. ESBL-producing organisms are resistant to a wide range of antibiotics, including penicillins, cephalosporins, and aztreonam, making infections caused by these bacteria challenging to manage. Understanding the nature of ESBL-producing bacteria and implementing effective strategies to reduce their spread are crucial for mitigating the risks associated with these pathogens.
Key Points
- ESBL-producing bacteria are a significant cause of antibiotic-resistant infections, necessitating careful management and prevention strategies.
- Hygiene practices, such as hand washing and environmental cleaning, play a critical role in reducing the spread of ESBL-producing organisms.
- Antibiotic stewardship programs are essential for minimizing the selective pressure that drives the emergence and dissemination of ESBL-producing bacteria.
- Screening for ESBL carriage upon hospital admission can help in early identification and isolation of carriers, thereby reducing the risk of transmission.
- Implementing contact precautions for patients known to be colonized or infected with ESBL-producing bacteria is a key component of infection control strategies.
Understanding ESBL-Producing Bacteria

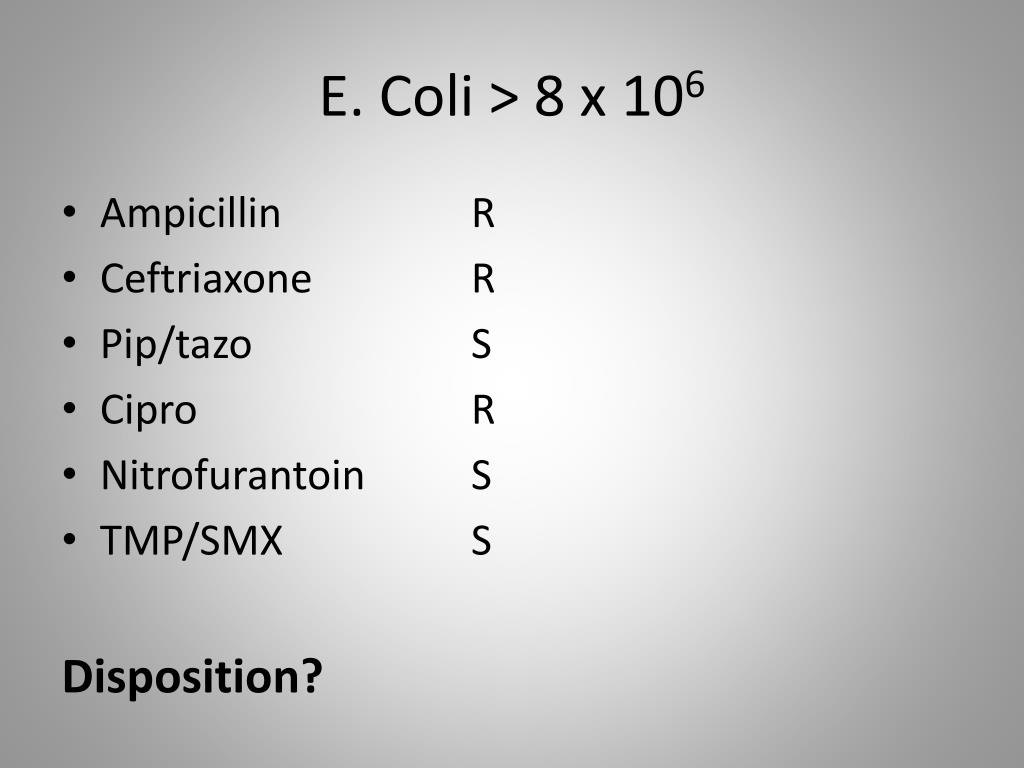
ESBL-producing bacteria are strains of bacteria that have developed resistance to a broad spectrum of beta-lactam antibiotics due to the production of ESBL enzymes. These enzymes can break down the beta-lactam ring of antibiotics, rendering them ineffective against the bacteria. The most common types of bacteria that produce ESBLs are Escherichia coli and Klebsiella pneumoniae, although other species can also be ESBL producers. The spread of ESBL-producing bacteria is facilitated by several factors, including antibiotic misuse, poor infection control practices, and the movement of patients between healthcare facilities.
Strategies for Reducing the Risk of ESBL Infections
Reducing the risk of ESBL infections requires a multifaceted approach that includes enhanced infection control measures, prudent use of antibiotics, and ongoing surveillance for ESBL-producing bacteria. Hand hygiene is a cornerstone of infection control and should be strictly adhered to by all healthcare workers. Environmental cleaning and disinfection are also critical, as ESBL-producing bacteria can survive on surfaces for extended periods. The implementation of antibiotic stewardship programs can help minimize the unnecessary use of antibiotics, thereby reducing the selective pressure that drives the emergence of resistance.
| Category | Strategy | Evidence of Effectiveness |
|---|---|---|
| Infection Control | Enhanced hand hygiene and environmental cleaning | Studies have shown significant reductions in the transmission of ESBL-producing bacteria with improved hygiene practices. |
| Antibiotic Use | Antibiotic stewardship programs | These programs have been associated with decreased rates of antibiotic resistance and reduced incidence of ESBL infections. |
| Surveillance | Screening for ESBL carriage upon hospital admission | Early identification of ESBL carriers can lead to targeted interventions and reduced transmission risk. |

Implementing Effective Infection Control Measures

Effective infection control is paramount in the prevention of ESBL infections. This includes contact precautions for patients known to be colonized or infected with ESBL-producing bacteria, which involves the use of gloves, gowns, and masks when interacting with these patients. Isolation of patients in single rooms can also help reduce the risk of transmission. Moreover, surveillance cultures can be an effective tool for identifying patients who are colonized with ESBL-producing bacteria, allowing for early intervention.
Role of Antibiotic Stewardship
Antibiotic stewardship programs play a vital role in reducing the risk of ESBL infections by promoting the appropriate use of antibiotics. These programs involve antibiotic use audits, feedback to prescribers, and the development of guidelines for antibiotic use. By minimizing unnecessary antibiotic use and ensuring that antibiotics are used appropriately, these programs can help reduce the selective pressure that drives the emergence of antibiotic-resistant bacteria, including ESBL producers.
In conclusion, reducing the risk of ESBL infections requires a multifaceted approach that includes enhanced infection control practices, prudent antibiotic use, and ongoing surveillance. By understanding the nature of ESBL-producing bacteria and implementing effective strategies to prevent their spread, healthcare providers can mitigate the risks associated with these pathogens and improve patient outcomes.
What are ESBL-producing bacteria, and why are they a concern in healthcare settings?
+ESBL-producing bacteria are strains of bacteria that have developed resistance to a wide range of antibiotics. They are a concern because they can cause infections that are difficult to treat, leading to prolonged hospital stays, increased healthcare costs, and higher mortality rates.
How can the spread of ESBL-producing bacteria be prevented in healthcare settings?
+The spread of ESBL-producing bacteria can be prevented through enhanced infection control measures, including hand hygiene, environmental cleaning, and contact precautions for patients known to be colonized or infected with these bacteria. Additionally, antibiotic stewardship programs can help minimize the unnecessary use of antibiotics.
What role do antibiotic stewardship programs play in reducing the risk of ESBL infections?
+Antibiotic stewardship programs play a critical role in reducing the risk of ESBL infections by promoting the appropriate use of antibiotics, minimizing unnecessary antibiotic use, and reducing the selective pressure that drives the emergence of antibiotic-resistant bacteria.