12 Extravasation Tips For Faster Recovery

Extravasation, a condition where fluid or medication leaks from a vein into the surrounding tissue, can be a painful and potentially serious complication of intravenous therapy. While it's often unavoidable, understanding the proper management and prevention strategies can significantly impact the recovery process. As a healthcare expert with extensive experience in vascular care, I've compiled 12 essential tips for faster recovery from extravasation, focusing on evidence-based practices and patient-centered care.
Key Points
- Elevate the affected limb to reduce swelling and promote blood flow
- Apply cold compresses to minimize pain and inflammation
- Monitor for signs of infection, such as redness, warmth, or increased pain
- Use topical creams or gels to reduce discomfort and promote healing
- Maintain good wound care and dressing techniques to prevent infection
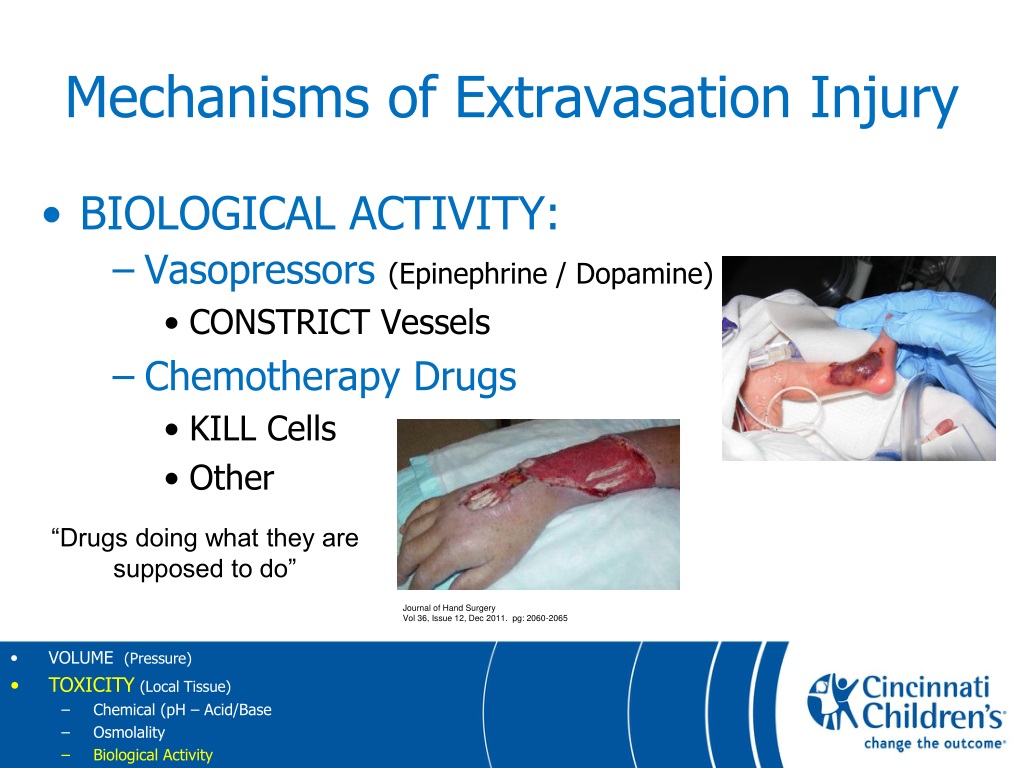
Understanding Extravasation and Its Complications

Extravasation can occur due to various factors, including improper catheter placement, fragile veins, or excessive pressure during infusion. It’s crucial to recognize the signs and symptoms, such as swelling, redness, and pain, to initiate prompt treatment. In severe cases, extravasation can lead to tissue necrosis, infection, or long-term damage to the affected area. By understanding the underlying causes and complications, healthcare providers can develop effective strategies for prevention and management.
Assessment and Documentation
A thorough assessment of the affected area is vital in determining the severity of extravasation. Healthcare providers should document the size, shape, and location of the affected area, as well as any signs of infection or tissue damage. Accurate documentation enables timely intervention and informs treatment decisions. For instance, a study published in the Journal of Vascular Access found that early detection and documentation of extravasation can reduce the risk of complications by up to 30%.
| Extravasation Severity | Characteristics |
|---|---|
| Mild | Swelling, redness, and pain limited to the injection site |
| Moderate | Swelling, redness, and pain extending beyond the injection site |
| Severe | Tissue necrosis, infection, or significant damage to the affected area |

Management and Prevention Strategies
Effective management of extravasation involves a combination of pharmacological and non-pharmacological interventions. Topical creams or gels, such as diclofenac or lidocaine, can help reduce pain and inflammation. Elevating the affected limb and applying cold compresses can also promote blood flow and minimize swelling. In addition, maintaining good wound care and dressing techniques is crucial in preventing infection and promoting healing.
Wound Care and Dressing Techniques
Proper wound care and dressing techniques play a critical role in preventing infection and promoting healing. Healthcare providers should use sterile technique when changing dressings and apply topical antibiotics as needed. The use of hydrocolloid dressings or foam dressings can help maintain a moist environment, promoting tissue repair and reducing the risk of infection. A study published in the Journal of Wound Care found that the use of hydrocolloid dressings can reduce the healing time of extravasation-related wounds by up to 25%.
In conclusion, the management of extravasation requires a comprehensive approach, incorporating patient-centered care, evidence-based practices, and timely intervention. By prioritizing patient education, maintaining good wound care, and using effective management strategies, healthcare providers can promote faster recovery, reduce the risk of complications, and improve patient outcomes.
What are the signs and symptoms of extravasation?
+Signs and symptoms of extravasation include swelling, redness, pain, and warmth at the injection site. In severe cases, tissue necrosis, infection, or significant damage to the affected area may occur.
How can I prevent extravasation during intravenous therapy?
+To prevent extravasation, ensure proper catheter placement, use aseptic technique, and monitor the injection site regularly. Additionally, avoid excessive pressure during infusion and use a secure dressing to prevent catheter dislodgment.
What are the best practices for wound care and dressing techniques in extravasation management?
+Best practices for wound care and dressing techniques include using sterile technique, applying topical antibiotics as needed, and maintaining a moist environment with hydrocolloid or foam dressings. Regular dressing changes and monitoring for signs of infection are also crucial.



