Basal Insulin

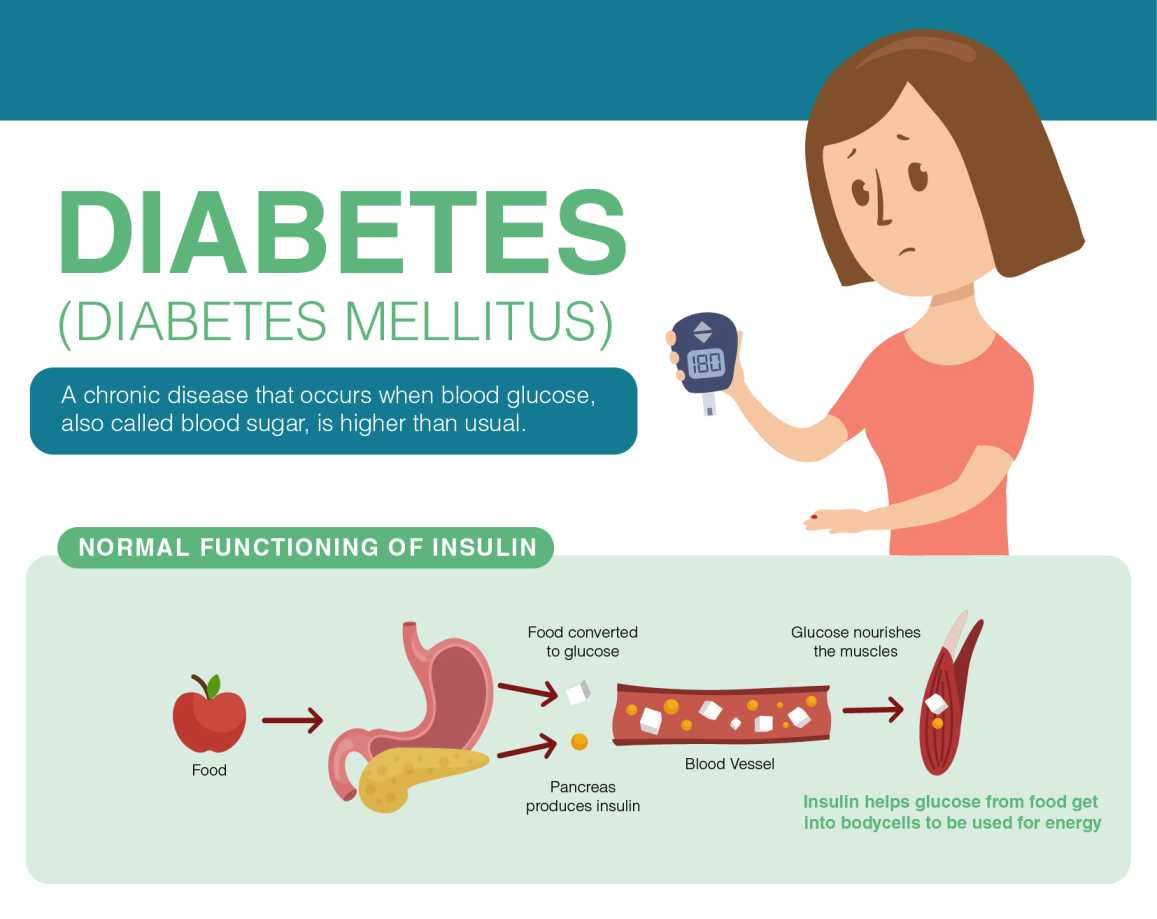
Basal insulin is a type of insulin that plays a crucial role in regulating blood glucose levels in the body. It is produced by the pancreas and works to control glucose levels between meals and during sleep. In individuals with diabetes, the body either does not produce enough insulin or is unable to effectively use the insulin it produces, leading to high blood glucose levels. Basal insulin therapy is often used to help manage these levels and prevent complications associated with diabetes. With a growing understanding of diabetes management, basal insulin has become a cornerstone in the treatment of both type 1 and type 2 diabetes.
The concept of basal insulin is rooted in the body's natural insulin production patterns. Normally, the pancreas produces two types of insulin: basal insulin, which is produced at a steady rate throughout the day, and bolus insulin, which is released in response to meals to manage the spike in blood glucose levels. Basal insulin analogs are designed to mimic the body's natural basal insulin production, providing a steady, background level of insulin throughout the day. This helps to control fasting blood glucose levels, reduce glucose variability, and improve overall glycemic control.
Key Points
- Basal insulin is crucial for regulating blood glucose levels between meals and during sleep.
- It is used in the treatment of both type 1 and type 2 diabetes to manage blood glucose levels.
- Basal insulin analogs are designed to mimic the body's natural basal insulin production.
- Effective basal insulin therapy can reduce the risk of diabetes-related complications.
- Personalized basal insulin regimens are essential for achieving optimal glycemic control.
Understanding Basal Insulin Therapy

Basal insulin therapy involves the administration of basal insulin analogs, which are modified versions of human insulin designed for prolonged action. These analogs can be administered via injection or, in some cases, through an insulin pump. The goal of basal insulin therapy is to maintain a steady level of insulin in the bloodstream, mimicking the body’s natural insulin production and thereby controlling fasting blood glucose levels. By achieving tight glycemic control, individuals with diabetes can reduce their risk of developing long-term complications such as cardiovascular disease, nephropathy, and retinopathy.
Types of Basal Insulin
There are several types of basal insulin analogs available, each with its own duration of action and onset of activity. The most commonly used basal insulins include glargine (Lantus, Toujeo), detemir (Levemir), and degludec (Tresiba). These insulins are characterized by their prolonged duration of action, allowing for once or twice daily dosing. For example, insulin glargine has a duration of action of approximately 24 hours, making it suitable for once daily administration. In contrast, insulin detemir has a slightly shorter duration of action and may be administered once or twice daily, depending on the individual’s needs.
| Basal Insulin Type | Duration of Action | Administration Frequency |
|---|---|---|
| Insulin Glargine (Lantus, Toujeo) | Approximately 24 hours | Once daily |
| Insulin Detemir (Levemir) | Approximately 16-20 hours | Once or twice daily |
| Insulin Degludec (Tresiba) | More than 42 hours | Once daily |
Implementing Basal Insulin Therapy
Implementing an effective basal insulin regimen requires careful consideration of several factors, including the patient’s current glucose control, lifestyle, and medical history. The initial dose of basal insulin is often determined based on the patient’s weight, with typical starting doses ranging from 0.1 to 0.2 units per kilogram per day. Adjustments to the dose are then made based on fasting glucose levels, with the goal of achieving target glucose levels without causing hypoglycemia. Regular monitoring of glucose levels and adjustment of the basal insulin dose as needed are crucial for achieving optimal glycemic control.
Monitoring and Adjusting Basal Insulin Doses
Monitoring fasting glucose levels is essential for adjusting basal insulin doses. Patients should aim to check their glucose levels at the same time each day, typically before breakfast, to assess the effectiveness of their basal insulin regimen. If fasting glucose levels are consistently above target, the basal insulin dose may need to be increased. Conversely, if levels are below target, the dose may need to be decreased to prevent hypoglycemia. It is also important to consider other factors that may affect glucose levels, such as changes in diet, physical activity, or other medications.
In addition to glucose monitoring, patients on basal insulin therapy should be aware of the signs and symptoms of hypoglycemia, which can include shakiness, dizziness, sweating, hunger, irritability, confusion, or difficulty speaking. If hypoglycemia occurs, it should be treated promptly with fast-acting carbohydrates, such as glucose tablets or juice, followed by a snack or meal to help stabilize glucose levels.
What is the primary goal of basal insulin therapy?
+The primary goal of basal insulin therapy is to maintain a steady level of insulin in the bloodstream, controlling fasting blood glucose levels and reducing the risk of diabetes-related complications.
How often should basal insulin be administered?
+Basal insulin can be administered once or twice daily, depending on the type of insulin and the individual's needs. The frequency of administration should be determined by a healthcare provider based on glucose monitoring data and other factors.
What are the potential side effects of basal insulin therapy?
+Potential side effects of basal insulin therapy include hypoglycemia, weight gain, and injection site reactions. Patients should be aware of these risks and monitor their glucose levels regularly to minimize the risk of complications.
In conclusion, basal insulin therapy is a critical component of diabetes management, offering individuals with type 1 and type 2 diabetes a means to achieve tight glycemic control and reduce their risk of long-term complications. By understanding the types of basal insulin available, implementing an effective basal insulin regimen, and monitoring glucose levels regularly, patients can work towards optimal diabetes management and improved overall health. As research continues to evolve, it is likely that new basal insulin formulations and delivery systems will become available, further enhancing the treatment options for individuals with diabetes.



